
START-SD is a federal program funded by the Health Resources and Services Administration (HRSA) working to increase access to and effectiveness of prevention, treatment, and recovery services for substance use disorder in South Dakota. It is a three-pronged project, with focuses on opioid use disorder, psychostimulant use disorder, and overdose response.
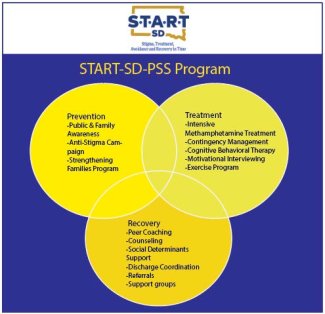
Psychostimulant use disorder is on the rise in South Dakota. The second prong of the START-SD project, START-SD-PSS, is designed to address barriers related to prevention, treatment, and recovery services for psychostimulant use disorder in four South Dakota counties: Brown, Codington, Hughes, and Roberts Counties. These four counties account for approximately 95,000 people, 2.5% of whom are at risk for illicit drug use. All four counties are rural counties and all four have been designated as mental health shortage areas with limited access to mental health services including treatment, counseling, and recovery.
Project team members from South Dakota State University have partnered with South Dakota Urban Indian Health (SDUIH) in Pierre, Avera St. Mary’s in Pierre, Avera St. Luke’s in Aberdeen, Coteau Des Prairies Health Care System in Sisseton, and Face-It TOGETHER, which is based in Sioux Falls. By working with these organizations and providers, the START-SD-PSS team will achieve its objectives.
Key Objectives
Objective 1:
Develop and distribute culturally and linguistically appropriate education materials designed to: (1) Improve family members’, caregivers’, and the public’s understanding of evidence-based prevention, treatment, and recovery strategies psychostimulant misuse and use disorders; and (2) Reduce stigma associated with the disease.
Objective 2:
Provide professional development to community partners to identify and screen individuals at risk for SUD including psychostimulant disorders and provide or make referrals to available prevention, harm reduction, early intervention, treatment, and other support services to minimize the potential for the development and adverse outcomes relate to psychostimulant disorders.
Objective 3:
Provide high-risk patients, with a focus on people who inject drugs, and their family members at treatment centers and community organizations with education on risks of developing infections including HIV, viral hepatitis, and endocarditis and the available resources for referrals to screening and treatment in the target counties.
Objective 4:
Recruit, train, and mentor interdisciplinary teams of SUD/OUD clinical and social service and community-based providers who are able to identify and treat psychostimulant misuse and use disorders using evidence-based methods.
Objective 5:
Enhance discharge coordination for people in treatment and recovery and/or leaving the criminal justice system who require linkages to home and community-based services and social supports with the goal of improving health care in target rural areas.
Objective 6:
Expand peer workforce and programming as interventionists in various settings, including hospitals, emergency departments, law enforcement departments, jails, SUD/OUD treatment programs, and in the community.
Objective 7:
Support the development of recovery communities, recovery coaches, and recovery community organizations that are utilizing culturally centered approaches, with a focus on Native American cultural practices, in Hughes and Roberts Counties.
Contingency Management
The implementation of contingency management programs has been a key element of the psychostimulant use disorder focus of START-SD. Contingency management is an addiction treatment method that encourages patients to meet their treatment goals through incentives.
For contingency management to be effective, it needs to be personalized for the patient. Caregivers work individually with patients to determine appropriate goals based on where the patient is in their treatment and to select worthwhile incentives.
Through START-SD, we hope to set up contingency management programs throughout the state. Coteau des Prairies Health Care System in Sisseton, South Dakota will be leading the way for the implementation of contingency management through START-SD.
This work is being completed with the help of our key partners
South Dakota Urban Indian Health is a non-profit corporation that operates two Federally Qualified Health Centers and Patient Centered Medical Homes, providing medical, behavioral health, and cultural services in Sioux Falls and Pierre. The Pierre clinic offers mental health and substance use disorder counseling services to patients of all ages, with the Tiospaye’ program providing holistic care for patients. SDUIH’s mission is: “to provide total quality medical care for Native American people and the economically disadvantaged residing in Urban areas of South Dakota. Care provided is not limited to just the medical needs but to provide holistic quality care for the entire family. Physical and mental healthcare are essential for a healthy society.”
Avera St. Mary’s is a comprehensive health care and medical specialty services system serving central South Dakota through their Pierre, SD location. They offer outpatient mental health, addiction treatment, and counseling services including comprehensive assessment services, individualized treatment planning, supportive therapy, intervention groups and relapse prevention to help patients achieve the best results for their unique situation. Avera’s mission is “to make a positive impact in the lives and health of persons and communities by providing quality services guided by Christian values.”
Avera St. Luke’s is a comprehensive health care and medical specialty services system serving northeastern South Dakota through their Aberdeen, SD location. They offer inpatient behavioral health programs for children, adolescents, and adults including intensive inpatient and methamphetamine treatment programs. Additionally, they offer outpatient mental health, addiction treatment, and counseling services including comprehensive assessment services, individualized treatment planning, supportive therapy, intervention groups and relapse prevention to help patients achieve the best results for their unique situation. Avera’s mission is “to make a positive impact in the lives and health of persons and communities by providing quality services guided by Christian values.”
Coteau des Prairies provides a wide range of health care services to the Sisseton, SD community and surrounding area in northeastern South Dakota. Through the Compass Care program, they provide medical, social and mental health care including SUD treatment, Medication-Assisted Treatment and care coordination. CDP’s mission: “we are passionate about the work we do. We believe in offering our patients individualized attention and care, emphasizing their unique needs and treating them as individuals on a human level. We have been successful in this goal, with patient satisfaction scores ranking in the top 3% nationwide! Simply put, our mission is to provide: Quality Care with a Personal Touch, Close to Home.”
Face It TOGETHER is a nationally-focused addiction wellness nonprofit that provides professional peer coaching to those impacted by addiction, including loved ones. Their mission is to get people with addiction and their loved ones well. By pairing members (clients) with coaches who have similar lived experiences, they are welcomed into a safe, nonjudgmental space where they can begin to overcome the challenges in their lives related to addiction. Coaches meet members at any point in their journeys. They offer guidance in a personalized way. Members don’t have to follow a one-size-fits-all program or remain sober to stay engaged with a FIT coach.
Project Manuscripts
Funding Statement
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $500,000 with 100% percentage funded by HRSA/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA/HHS or the U.S. Government. More Information
Project Directors

Erin Miller
Interim Center Director, Community Practice Innovation Center (CPIC), Assistant Professor, Department of Allied and Population Health
Department of Allied and Population Health
Community Practice Innovation Center
College of Pharmacy and Allied Health Professions
SDSU - Sioux Falls

Faculty

Jeremy Daniel
Associate Professor
College of Pharmacy and Allied Health Professions
Department of Pharmacy Practice
Community Practice Innovation Center

Christopher Robbins
Assistant Professor
Department of Allied and Population Health
Community Practice Innovation Center
Support Team

Irene Arango Gomez
Community Care Coordinator
Department of Allied and Population Health
College of Pharmacy and Allied Health Professions


